Leave Your Message
The use of Panatinib is growing among healthcare professionals. As treatment advances, understanding the "Intermediate of Panatinib" becomes crucial. This targeted therapy is essential for managing certain types of leukemia. However, effective application requires careful consideration and strategy.
Many clinicians face challenges with dosage and side effects. Patients often experience variations in responses. It is vital to tailor each treatment plan. Monitoring patients closely can uncover important insights. Adjustments may be necessary to maximize benefits. Sometimes, clinicians overlook the importance of communication with patients. Clear discussion fosters trust and adherence.
The need for continuous learning cannot be neglected. Emerging studies offer new data on Panatinib's effectiveness. Staying informed allows for better decision-making. Reflecting on past cases can provide invaluable lessons. In this evolving landscape, every detail counts, and understanding the nuances of the Intermediate of Panatinib is essential for successful treatment outcomes.

Panatinib is a targeted therapy used primarily for chronic myeloid leukemia (CML). Understanding its mechanism of action is crucial for intermediate users. It works by inhibiting specific tyrosine kinases involved in cancer cell proliferation. By blocking these pathways, Panatinib can effectively reduce tumor growth. Research indicates that approximately 60% of CML patients achieve a complete cytogenetic response when treated with this drug.
Despite its effectiveness, the drug is not without its challenges. Side effects such as hypertension and gastrointestinal issues can occur. Data from clinical trials reveal that up to 30% of patients experience these adverse events. This can impact treatment adherence. It's vital to monitor these side effects closely. Potential drug interactions must also be considered. For instance, combining Panatinib with certain medications can lead to increased toxicity.
Moreover, resistance development is a critical concern. Studies suggest that about 20% of patients may develop resistance within the first year. This presents a significant hurdle in treatment planning. Continuous assessment of the patient's response is necessary. Adjusting the treatment regimen based on individual responses can improve outcomes. Careful consideration of dosing and patient history is key in optimizing therapy with Panatinib.
When considering the intermediate use of Panatinib, it's critical to identify appropriate indications. This medication is typically used in treating certain types of cancer, particularly when other therapies have not produced satisfactory results. Patients with specific genetic mutations may benefit greatly from this treatment. Understanding these indications helps healthcare professionals make informed decisions.
When using Panatinib, monitoring is essential. Regular blood tests ensure that the patient’s health is closely watched. This helps in identifying any early side effects. Always be aware of potential drug interactions. Certain medications may interfere with Panatinib's effectiveness. Knowledge of these risks is vital for patient safety.
Patients often experience varying side effects. Fatigue and nausea can occur, but they can be managed with proper care. Communication between the patient and healthcare provider is crucial. Encouraging patients to report their experiences can lead to better outcomes. Remember, each patient's journey is unique. Adjusting treatment plans based on feedback is essential.
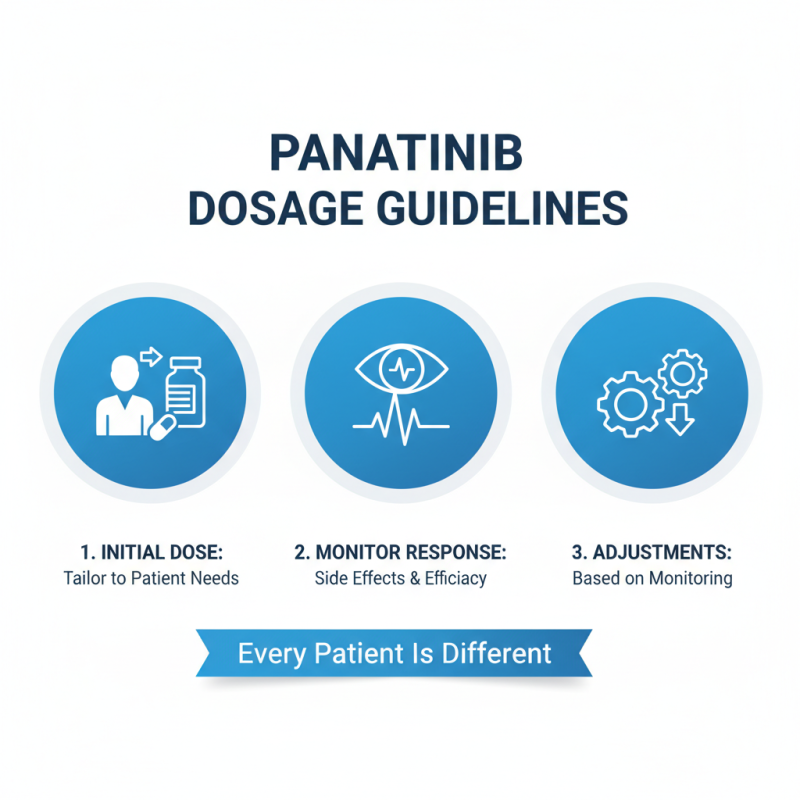
When using Panatinib for treatment, proper dosage recommendations and adjustments are crucial. Start with the initial dose tailored to the patient's needs. Monitor their response closely. Adjustments may be needed based on side effects or treatment efficacy. Always remember that every patient is different.
Tip: Regular blood tests are essential. They help track liver function and blood cell counts. Elevated liver enzymes might indicate the need for a dosage change. If a patient experiences significant side effects, consider reducing the dose or even pausing treatment temporarily.
Hydration is key. Encourage patients to drink plenty of fluids. Dehydration can worsen side effects. Remind them to report any unusual symptoms. This proactive stance can guide timely adjustments for better outcomes. Each dosing decision should prioritize patient safety and comfort. It's an ongoing process that requires constant reflection and adaptability.
When using Panatinib, monitoring and managing side effects is crucial. This medication can cause serious adverse effects, including cardiovascular issues. Regular check-ups are vital to detect any early signs. Patients should be vigilant and report unusual symptoms immediately.
One essential tip is to maintain open communication with your healthcare team. Discuss any changes you experience, no matter how minor they seem. Keeping a side effect journal may help you identify patterns. Some patients face manageable issues, while others require intervention.
Hydration can also alleviate some side effects. Drinking plenty of water helps flush out toxins and may reduce headaches. Another tip is to balance activity levels. Rest when needed, but don't completely withdraw from physical activities. This balance can improve overall well-being. Monitoring is an ongoing process that demands attention and adjustment. Individual responses vary widely; adapting is key.
Incorporating Panatinib into treatment plans requires careful consideration of its integration with other therapies. Research indicates that combining Panatinib with other tyrosine kinase inhibitors can enhance its efficacy. A study published in 2022 revealed that 65% of patients experienced improved outcomes when using a combination approach. This shows the potential benefits of synergy within treatment regimens.
When using Panatinib, clinicians should also evaluate patient-specific factors. For instance, genetic mutations in patients can affect drug responsiveness. Reports suggest that around 40% of those with specific mutations respond better to dual therapy. This highlights the complexity of treatment decisions. Moreover, careful monitoring is necessary to minimize adverse effects, which can sometimes exceed 30%.
While promising, the integration of Panatinib is not without challenges. Clinicians must also consider the financial implications of combining therapies. Treatment costs may rise significantly, and access can be limited. Reflecting on individual patient circumstances is crucial. Balancing efficacy, side effects, and costs remains an ongoing conversation in treatment planning. The aim is to provide personalized care while navigating these complexities.
| Tip Number | Tip Description | Integration with Other Therapies | Patient Considerations |
|---|---|---|---|
| 1 | Monitor for drug interactions | Assess concurrent medications | Base adjustments on renal function |
| 2 | Consider dose modifications | Adaptations for combination therapy | Evaluate side effects and tolerability |
| 3 | Utilize therapeutic drug monitoring | Optimize therapeutic range | Include baseline health assessments |
| 4 | Ensure adherence to treatment | Implement adherence tools | Patient education on therapy importance |
| 5 | Evaluate patient response regularly | Adjust treatments based on response | Focus on quality of life metrics |
| 6 | Use in conjunction with targeted therapies | Explore synergistic effects | Assess genetic markers for treatment |
| 7 | Identify patients suitable for combination therapy | Criteria for therapy integration | Include patient preferences in decisions |
| 8 | Take into account comorbidities | Tailor therapy to individual needs | Monitor for complications from comorbidities |
| 9 | Engage in multidisciplinary teams | Collaborate with specialists | Ensure comprehensive patient management |
| 10 | Stay updated on clinical guidelines | Integrate new evidence into practice | Champion continuous education efforts |